Dr. Nowrouzi is a specialist in all types of new generation lamellar corneal transplantation, such as deep anterior lamellar keratoplasty (DALK), Descemet's membrane endothelial keratoplasty (DMEK), and Descemet's stripping automated endothelial keratoplasty (DSAEK).
Descemet's membrane endothelial keratoplasty (DMEK) is a partial thickness corneal transplant in which Descemet's membrane (DM) and host endothelium are replaced by DM and donor endothelium.
This is different from Descemet's stripping automated endothelial keratoplasty (DSAEK), where the donor MD, endothelium and posterior stroma replace the host MD and endothelium. DMEK and DSAEK are endothelial keratoplasty procedures, in contrast to a full-thickness penetrating keratoplasty (PK).
Endothelial keratoplasty procedures are not suitable for patients with healthy corneal endothelium, such as patients with stromal scarring or keratoconus. These patients still require DALK or PK.
Good candidates for DMEK

- Fuchs' endothelial dystrophy
- Posterior polymorphous membrane dystrophy
- Congenital inherited endothelial dystrophy
- Bullous keratopathy
- Iridocorneal endothelial syndrome (ICE)
- Failed endothelial keratoplasty
Unsuitable or very complex scenarios for DMEK

- Stromal healing
- Keratoconus
- Inability to lie down
- hypotonia
- aphakia
- Aniridia or large iris defects
- Anterior chamber intraocular lens
- Previous glaucoma surgery
- Risk of tissue loss through tubes, trabeculectomies or peripheral iridectomies
- Postoperative gas bubble leakage may occur with subsequent graft detachment.
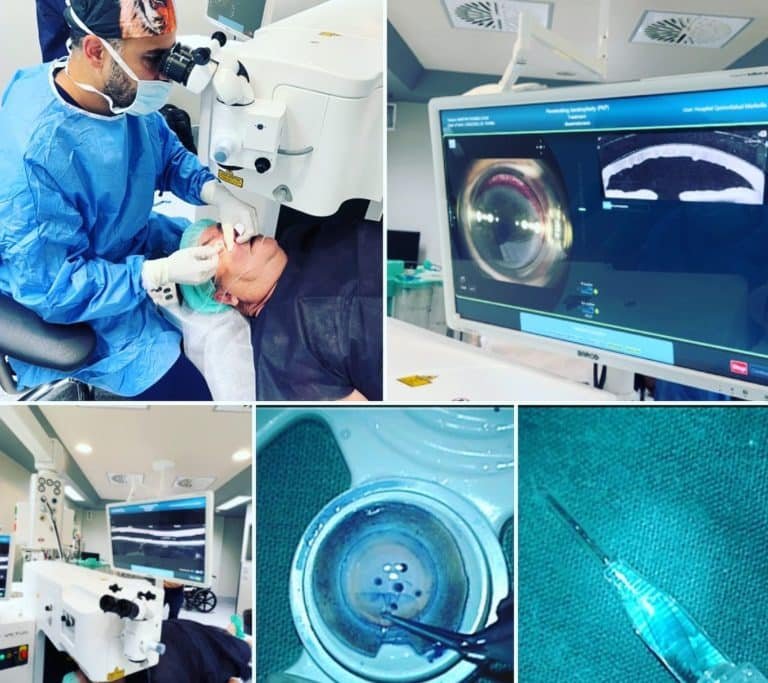
DMEK is a relatively new procedure and surgeons continue to develop many new and exciting techniques and strategies. Nowrouzi, through new technologies, such as the use of real-time intraoperative OCT and femtosecond laser with DMEK, offers these new generation technologies to its patients.

Eye banks are likely to continue to play an important role in DMEK surgery and their - removal of DMEK tissue reduces tissue attrition by the surgeon during preparation. Improving the number and viability of endothelial cells should remain an important research focus.
Descemet's membrane endothelial transfer gene therapy or Rho-associated kinase inhibitors are particularly interesting areas where Dr. Nowrouzi first initiated these new treatments in the region and offers all these new generation therapeutic approaches to his patients.
Advantages of DMEK over DSAEK
DMEK has been shown to have superior visual outcomes compared to DSAEK. In multiple studies in which patients had DSAEK in one eye and DMEK in the other eye, significantly better visual acuity and preferences were reported in the DMEK eye.
Guerra et al. reported better corrected visual acuity in a DMEK group at 1 year of 20/24 compared to 20/32 in a DSAEK group. The 85% reported better quality of vision in the DMEK eye. Endothelial cell loss at 1 year was 1 % in DMEK eyes and 31 % in DSAEK eyes.
However, some studies suggest that the visual results of DSAEK can be improved with ultrathin tissue. Although recovery is slower with ultrathin DMEK than with DMEK, the final visual results after 1 year are comparable.
If the ultra-thin DSEK technique continues to improve, its ease and reliability may decrease the use of DMEK.
DMEK also has a lower immunological rejection rate and has the advantage of using a smaller incision (2.8 mm) than DSAEK (5 mm).