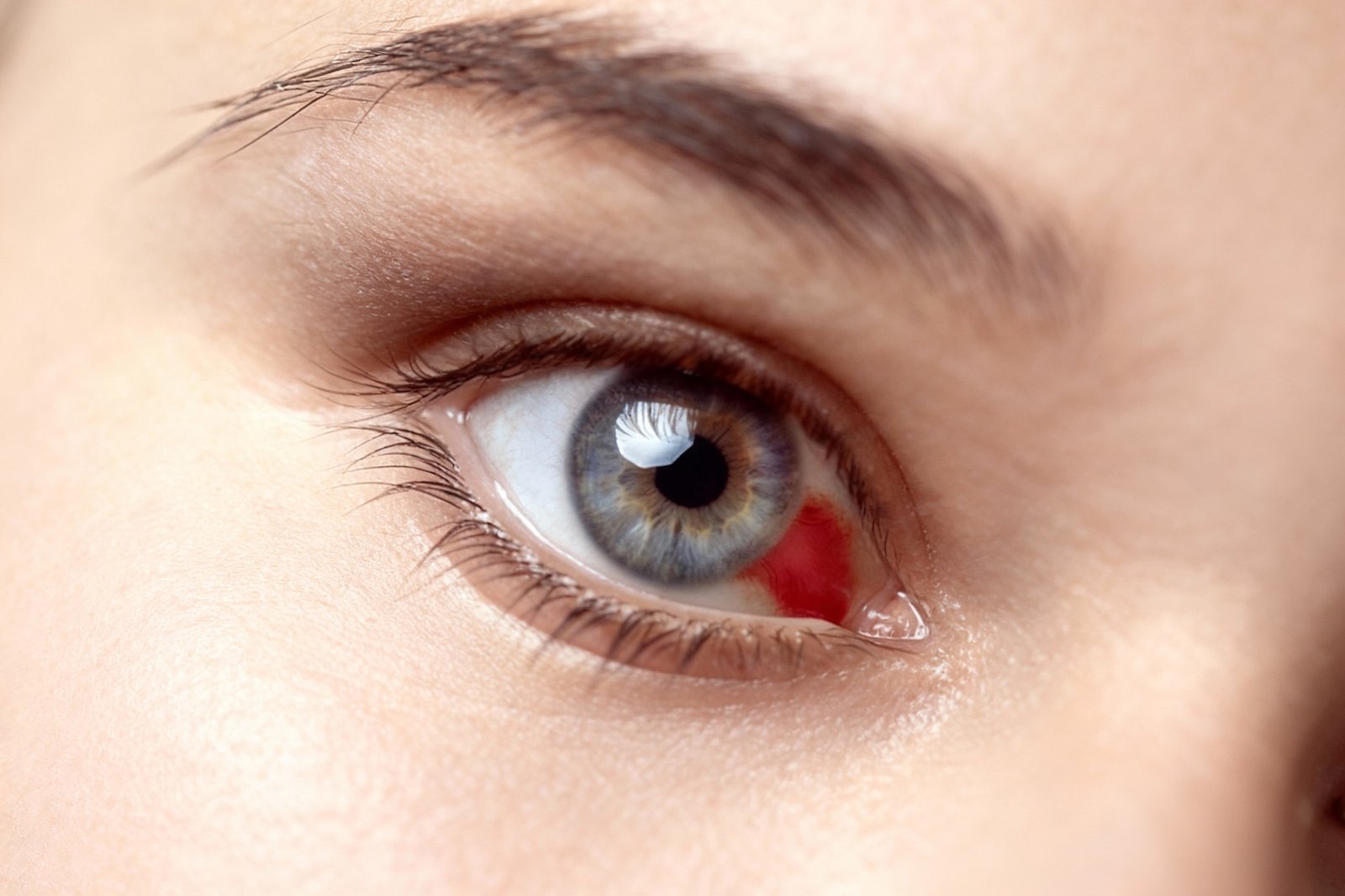
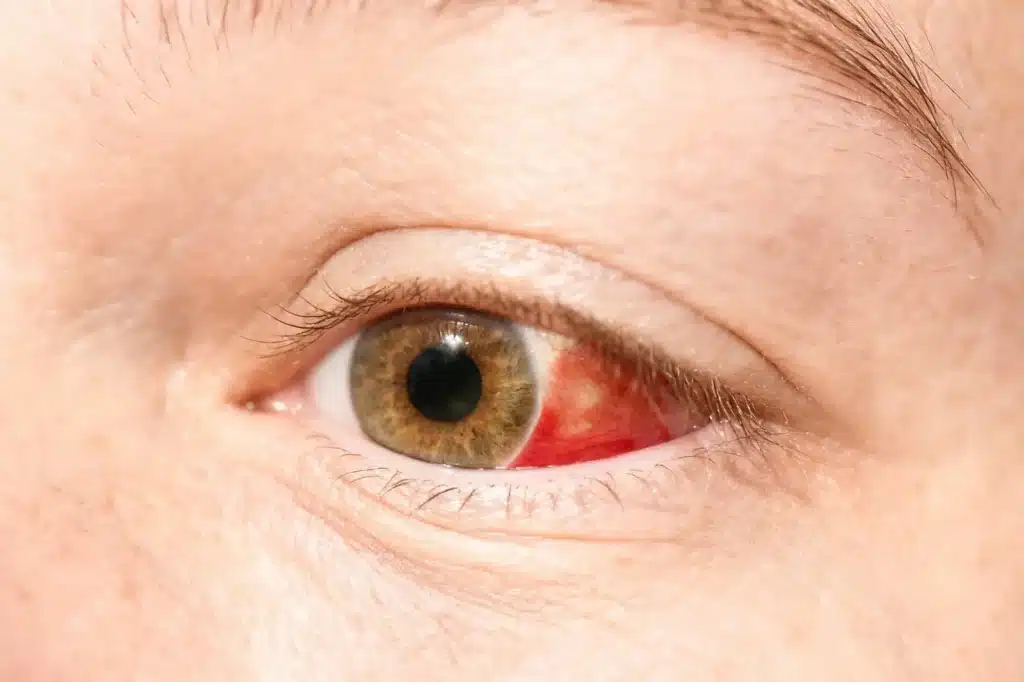
Eye effusion, known as subconjunctival haemorrhage, presents as a red spot in the white part of the eye. This condition is usually benign and does not cause pain or affect vision. It can be caused by a variety of factors, such as trauma, variations in blood pressure, systemic diseases and the use of certain medications. Although it is not usually serious, it is important to be aware of its symptoms and when it is necessary to consult a specialist.
What is an ocular effusion?
This term is used to describe a eye condition which causes alarm to patients, despite its generally benign nature.
Definition and characteristics
The subconjunctival haemorrhage is a collection of blood in the space between the conjunctiva and the sclera, the white part of the eye. It presents as a bright red spot visible to the naked eye. This condition results from the rupture of small blood vessels, allowing blood to leak under the conjunctiva. Despite its unusual and alarming appearance, subconjunctival haemorrhage usually does not cause pain or affect vision, and tends to resolve spontaneously within 10 to 15 days.
Differences with other eye problems
Subconjunctival haemorrhage can be confused with other eye conditions. However, its distinctive features allow it to be differentiated from other diseases. Here are some key differences:
- Subconjunctival haemorrhage vs. conjunctivitisConjunctivitis usually presents symptoms of itching, irritation and discharge, while ocular effusion lacks these symptoms.
- Subconjunctival haemorrhage vs. uveitisUveitis can lead to eye pain and impaired vision, unlike haemorrhage which is painless and does not affect visual acuity.
- Subconjunctival haemorrhage vs. glaucomaGlaucoma is associated with increased intraocular pressure and involves symptoms such as blurred vision and pain. Ocular effusion does not produce these symptoms.
- Subconjunctival haemorrhage vs. retinal detachmentSubconjunctival haemorrhage is a medical emergency and presents with symptoms such as shadow vision or flashes of light. Subconjunctival haemorrhage does not have these associated signs.
The differences allow ophthalmologists to make a proper diagnosis, ensuring that the patient receives the necessary care for their specific case. Careful observation of the characteristics of the eye effusion helps to rule out other ocular complications that may require immediate treatment.
Have you got a red spot in your eye and don't know if it's serious? We will assess you in less than 48 hours and you will leave with a clear plan. Book your appointment.
Causes of ocular effusion
There are different factors that can cause an eye effusion. Understanding the causes is essential in order to address the appropriate treatment and prevent future occurrences.
Trauma and injuries
Injuries or blows to the eye area are one of the most common reasons for an eye effusion. Direct contact, such as a blow or fall, can rupture the small blood vessels in the conjunctiva. Also, excessive rubbing or rubbing of the eye can result in an effusion, especially if done with force or in a state of eye irritation.
Variations in blood pressure
Drastic changes in blood pressure can trigger the rupture of capillaries in the eye. Events such as sneezing, intense coughing, physical exertion when lifting heavy objects or episodes of vomiting are associated with this type of ocular haemorrhage. This phenomenon is often related to Valsalva manoeuvres, which occur during exertion or stress.
systemic diseases such as hypertension and diabetes
Certain health conditions can influence the likelihood of experiencing eye effusions. High blood pressure is notably common among those who suffer from these episodes. A significant increase in blood pressure can lead to ruptured blood vessels in the conjunctiva. Similarly, patients with diabetes are at high risk, as this disease can adversely affect eye health.
Use of anticoagulant drugs
Treatment with drugs that affect blood clotting increases the likelihood of suffering an eye stroke. Drugs such as anticoagulants and some analgesics such as acetylsalicylic acid or ibuprofen have been associated with ruptured capillaries. Their use may increase the risk of subconjunctival haemorrhages, which should be considered when assessing eye health.
Eye infections and procedures
Infections affecting the eye area can contribute to the development of effusions. Some viral diseases that affect the eyes, along with respiratory infections that cause coughing and sneezing, pose an added risk. Also, after certain eye procedures, such as surgery or laser treatments, an increased incidence of subconjunctival haemorrhages may be observed.
Stress and its influence on eye health
Stress may play a role in eye health, although the relationship is less clear. Sudden changes in blood pressure caused by situations of high mental or physical stress may be a contributing factor to the occurrence of strokes. However, it is important to note that the connection between stress and eye strokes is still being studied and is not fully established.
Symptoms of ocular effusion
The presence of an eye effusion manifests itself primarily through visible symptoms, but there may also be less obvious signs that require attention. It is essential to be aware of these symptoms in order to identify the situation properly.
Identification of visible and invisible symptoms
One of the most noticeable signs of an eye effusion is the appearance of a bright red spot on the white of the eye. This spot can vary in size from a small patch to a wider coverage of the sclera. The absence of pain often characterises this type of haemorrhage, which may lead many to consider it a minor problem.
On the other hand, not all manifestations are visible. In some cases, the patient may experience:
- Slight irritation or foreign body sensation in the eye.
- Mild discomfort when blinking.
- Reduced sensitivity to light, but no significant change in vision.
Most of these invisible symptoms do not represent an imminent danger but require attention to rule out other serious eye conditions that may be at play.
When to consider dangerous ocular effusion
Although eye effusion is usually benign, there are circumstances in which it is crucial to seek medical attention. Particular attention should be paid to the following scenarios:
- Presence of significant eye pain, which is not relieved with time.
- Changes in vision, such as blurred vision or loss of part of the visual field.
- Recurrent ocular drifts that occur for no apparent reason.
- Situations involving major trauma to the eye area.
Early recognition of these symptoms can be vital to avoid further complications. Consultation with an ophthalmologist is essential in these cases to make a proper diagnosis and prevent possible long-term damage.
Diagnosis of ocular effusion
Diagnosis of an eye effusion is essential to determine its origin and to ensure that there are no underlying complications. Proper diagnosis allows for appropriate treatment and effective eye health care.
Clinical evaluation by the ophthalmologist
The first stage of diagnosis involves a thorough clinical evaluation by an ophthalmologist. During the consultation, the specialist will examine the affected eye using a slit lamp, an instrument that allows close observation of ocular structures. This evaluation includes several aspects:
- Visual inspection of subconjunctival haemorrhage.
- Determination of the extent and size of the red spot.
- Analysis of general eye health, assessing the presence of other associated problems or symptoms.
Doctors will also inquire about the patient's medical history, focusing on recent events such as trauma or variations in blood pressure, as well as any medications being taken. This information is essential to formulate an accurate diagnosis.
Additional diagnostic tests
While clinical evaluation usually provides the necessary information, in certain cases additional tests may be required. These tests help to rule out other eye or systemic conditions that could be causing the effusion. Some of the possible tests include:
- Ocular ultrasoundIt is used to examine internal structures of the eye to detect possible abnormalities that are not visible externally.
- Optical coherence tomography (OCT)This test provides detailed images of the layers of the retina and can reveal problems associated with ocular haemorrhage.
- Laboratory testsIn certain situations, blood tests may be ordered to evaluate coagulation problems or systemic diseases that could influence eye health.
The ophthalmologist, after interpreting the test results, will be able to provide a clear diagnosis and plan appropriate treatment, thus ensuring the best possible care for the patient.
Treatment of ocular effusion
Management of ocular effusion focuses on providing comfort and ensuring that there are no complications. Although the condition usually resolves on its own, there are several measures that may be helpful during the recovery process.
If the effusion recurs or you are taking anticoagulants, your case should be reviewed. Ask for an ophthalmological assessment.
Initial measures and basic care
In most cases, it is recommended to avoid any kind of friction or pressure on the affected eye. This includes not rubbing the eye or trying to touch the area. Keeping the area clean and, if necessary, using cold compresses can help relieve any feelings of irritation. Maintaining adequate eye hydration is also essential.
- Avoid wearing contact lenses until the effusion has resolved.
- Do not expose to dusty or heavily polluted environments to prevent further irritation.
- Limit strenuous physical activity during the healing period.
Use of artificial tears and other treatments
Artificial tears can be helpful in relieving dryness and irritation in the affected eye. These types of eye lubricants help to maintain moisture and relieve discomfort. However, they do not speed up the reabsorption of accumulated blood.
In situations where there is significant irritation or discomfort, the doctor may recommend the use of anti-inflammatory medication in the form of drops. It is important to follow up with the practitioner to tailor the treatment according to the needs of each case.
Possible need to discontinue anticoagulant treatment
For patients who are on a regimen of anticoagulants, it is essential to contact the doctor at the onset of an eye effusion. In some cases, the specialist may assess the possibility of adjusting the medication, especially if the stroke is recurrent or if there are other associated risk factors.
It will always be the physician who determines the best approach in these cases, taking into account the benefits and risks of treatment in the context of the patient's overall eye health.
When to consult a specialist
Medical attention in the event of an ocular effusion is essential to ensure visual health. There are certain situations in which it is imperative to seek the opinion of a qualified professional.
Urgency criteria
It is vital to be aware of signs that may indicate the need for immediate medical attention. Some of the situations that require urgent contact with an ophthalmologist include:
- Eye haemorrhages or effusions accompanied by severe pain.
- The occurrence of an ocular effusion following significant trauma to the eye.
- Alterations in vision, such as partial or total loss of vision.
- Presence of abnormal discharge or severe irritation of the eye.
- Development of additional symptoms such as severe headache or nausea, which may suggest a systemic complication.
Specialised care for patients with pre-existing conditions
Individuals suffering from chronic medical conditions should be particularly cautious. Those with a history of hypertension or diabetes may be more susceptible to complications and should consider the following:
- If eye leakage occurs frequently, it could be a sign of an underlying problem in the vascular system.
- Fluctuations in blood pressure may be manifested by subconjunctival haemorrhages.
- Patients on anticoagulant drugs should be monitored for any bleeding, as they may be at increased risk.
Regular ophthalmological assessment is essential for these patients, as it can help prevent serious complications related to their eye health. Therefore, it is advisable that they consult immediately upon the onset of an ocular effusion, as proper management of their pre-existing conditions can be key to avoiding additional risks. Early diagnosis and treatment are essential to maintain the integrity of your eye health.
Prevention and preventive care
The adoption of preventive measures is key to reducing the incidence of eye effusions. This care focuses on the control of risk factors, as well as the importance of regular ophthalmological check-ups.
Control of risk factors
Proper management of several factors can minimise the chances of subconjunctival haemorrhage. Some of the most relevant aspects are detailed below:
- Blood pressure monitoring: Keeping hypertension under control is essential. Regular check-ups and following medical indications for treatment are suggested.
- Management of systemic conditions: For those with diabetes, proper control of glucose levels is vital. Eye health can be affected by fluctuations in these levels.
- Prudent use of medications: Some people may be under treatment with anticoagulants or medications that affect clotting. It is essential to inform the doctor about any medication being taken.
- Avoiding trauma: Precautions when performing activities that involve risk to the eyes, such as contact sports or inappropriate handling, are vital. The use of eye protection is recommended in appropriate situations.
- Stress management: Practising relaxation techniques and stress management strategies can help regulate blood pressure and consequently decrease the risk of vascular ruptures.
Importance of regular eye examinations
Regular eye care is essential to maintain eye health. Check-ups allow problems to be detected before they become more serious.
Follow-up visits should be tailored to the needs of the individual patient, especially for those with pre-existing conditions. The following points are recommended:
- Frequency of visits: Patients with risk factors, such as hypertension or diabetes, should schedule more frequent check-ups. In general, an annual visit is appropriate for healthy adults.
- Comprehensive evaluations: Comprehensive evaluations including vision tests and eye pressure checks should be carried out during check-ups.
- Symptom education: Ophthalmologists can provide guidance on warning signs and symptoms that may require immediate attention.
Close attention and accurate diagnoses with state-of-the-art technology. Consultation agenda with Dr. Nowrouzi.